Nephron
The kidneys are the primary organs of excretion removing nitrogenous wastes. It is made up of nephrons which form urine. In this topic, we will see in detail the nephron function and mechanism of urine formation.
Definition
Nephron: It is the structural and functional unit of the kidney each capable of forming urine.
Importance
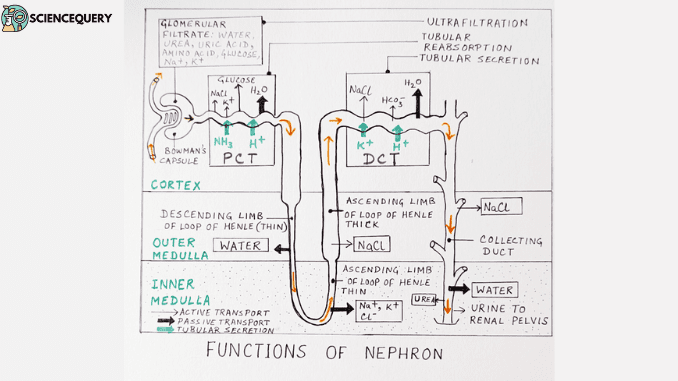
The different parts of the nephron are specialized to perform the following processes which lead to urine formation.
- Glomerular Filtration or ultrafiltration in the Malpighian capsule
- Tubular Reabsorption in the Proximal convoluted tubule (PCT)
- Tubular secretion in the Distal convoluted tubule (DCT)
Kidney Importance and Function
A pair of kidneys are there in the human urinary system. It is the main excretory organ. All nitrogenous wastes are excreted by the kidney in the form of urine. The various functions of the kidney are :
- Excretion of nitrogenous wastes
- Osmoregulation and homeostasis
- Regulation of blood pressure
- Regulation of electrolytes and salt concentration and pH
- Secretion of Renin and Erythropoietin production.
Nephron function and urine formation

A. Filtration in Glomerulus and Bowman’s capsule
The glomerular capillaries are narrower than the afferent arterioles. So the blood pressure in the glomerular capillaries is very high. This ensures a continuous process of ultrafiltration (filtration under pressure) through the glomerular capillaries.
- Hydrostatic pressure created by the glomerular blood is equivalent to 60 mm of Hg Pressure exerted by the plasma proteins in the glomeruli (which are not filtered) is 32 mm of Hg.
- Hydrostatic pressure exerted by the filtrate on the membrane of the Bowman’s capsule is 18 mm of Hg
- Net filtration pressure which promotes the process of ultrafiltration is 60-18-32= 10 mm Hg.
- This gives rise to the glomerular filtrate which contains large amounts of water and other dissolved substances sodium, potassium, chloride and bicarbonate ions, glucose, amino acid, urea, uric acid, creatinine, vitamins, and hormones.
B. Reabsorption in PCT
- Water is reabsorbed by osmosis from the tubular lumen to the renal interstitium through aquaporins or water channels.
- Sodium ions are absorbed through the primary active transport system into the peritubular capillary with the help of primary active transporters like sodium-potassium ATPase.
- Glucose and amino acids are fully reabsorbed into the peritubular capillary. The sodium glucose-linked transporter SGLT moves glucose against its concentration gradient. The process is called secondary active transport.
- SGLT binds two sodium ions and one glucose molecule from the tubular fluid and releases it inside the cell. From inside the cell, it is moved to the peritubular capillaries by special glucose transporters GLUT1 or GLUT2 a process known as facilitated transport.
- Chloride, potassium, and bicarbonate ions are also reabsorbed as it is important for maintaining the pH of the blood.
C. Reabsorption and secretion in Loop of Henle
- The upper thick segment of the descending limb of the loop of Henle is impermeable to water and ions. It just transfers the filtrate to the narrow segment of the descending limb. The lower thin segment of the descending limb is freely permeable to water and almost impermeable to electrolytes.
- So the water moves out into interstitial fluid by osmosis and the filtrate becomes hypertonic as sodium and other solutes are not reabsorbed here.
- The ascending limb of the loop of Henle’s lower thin segment is impermeable to water but permeable to potassium, chloride, and sodium ions.
- The upper thick segment of the ascending limb actively transports sodium chloride from filtrate to interstitial fluid in the medulla and the filtrate becomes hypotonic. The osmolarity of the interstitium becomes high.
- Urea is secreted in a very small amount into the thin ascending segment of the Loop of Henle.
D. Secretion in Distal Convoluted tubule (DCT)
- Potassium ions are secreted into the filtrate in DCT by active transport.
- Hydrogen, ammonium, and bicarbonate ions from the blood are secreted into the filtrate by active transport.
- Creatinine, hippuric acid, and pigments are also secreted from the blood into the filtrate here.
E. Reabsorption in collecting duct
- It plays a major role in maintaining the pH and ionic balance of blood by selective secretion of hydrogen and potassium ions.
- When water in the blood plasma goes down posterior pituitary releases ADH hormone. This increases the permeability of the collecting duct. Water is reabsorbed from the filtrate and concentrated urine in less volume is produced.
- When the water level of plasma is normal ADH secretion stops and the permeability of the collecting duct decreases. Less water is absorbed from the filtrate. This results in the production of more mount of dilute urine.
Hormonal regulation of Nephron function
ADH and its effect
| High osmotic pressure in blood is detected by osmoreceptors in the hypothalamus. | Low osmotic pressure in blood is detected by osmoreceptors in the hypothalamus. |
| Decreased water intake leads to low water content and a fall in the Glomerular filtration rate. | Increased water intake leads to high water content in blood and an increase in glomerular filtration rate. |
| Increased ADH circulation in blood leads to increased permeability of DCT and collecting duct. | Decreased ADH in circulation leads to decreased permeability of DCT and collecting duct. |
| Increased reabsorption of water from tubules into the bloodstream | Decreased reabsorption of water from tubules in the bloodstream. |
| Concentrated or hypertonic urine is produced | Dilute or hypotonic urine is produced. |
Renin Angiotensin Aldosterone system (RAAS)
- When the blood loses sodium ions it also loses water by osmosis. It results in low blood volume and blood pressure falls.
- This is detected by the JGA juxtaglomerular apparatus.
- It is located at the vascular pole of the nephron where afferent and efferent arterioles enter and leave the glomerulus.
- JGA operates a multihormonal RAAS to regulate the salt balance in the body. It is done in the following way.

Blood pressure regulation
- Another peptide hormone called Atrial Natriuretic Factor ( ANF) opposes the regulation by RAAS.
- It is done in the following way

Formation of urine
Composition of urine
- Human urine is 95% water and 5% other substances.
- Organic substances are mainly nitrogenous compounds comprised of urea, uric acid, creatinine, and hippuric acid.
- Non-nitrogenous organic compounds in urine are vitamins, enzymes, hormones oxalic acid.
- The inorganic substances include chloride, phosphate, potassium, sodium calcium, and magnesium.
- Pigments and drugs if taken are also present.
Characteristics of urine
- Urine is a transparent, yellow liquid and is slightly acidic with a specific gravity of 1.003 to 1.004 slightly heavier than water.
- The color of the urine is due to the presence of pigment urochrome.
- A normal adult person secretes about 1.5 liters of urine in 24 hours.
- It has a faint odor due to a substance urinod and on standing it smells of ammonia due to degradation of urea under bacterial activity. Glucose and other proteins are generally absent.
Role of Nephrons
The nephrons vary the volume and the composition of the urine day to day depending upon the diet and quantity of fluid intake by an individual.
Factors that affect urine formation
The factors that affect the urine formation are :
- Body fluid volume and composition; Dilute urine is formed when the body is hydrated and highly concentrated when the body is dehydrated due to various causes.
- The amount of urine output also varies with the time of the day, high during late morning and evening and reduces at night time.
- Intake of caffeinated drinks, and beverages increase the amount of urine output.
- A high-protein diet makes the urine hypertonic and loaded with urea.
- Diabetic individuals often produce urine loaded with glucose and the frequency of urination is also high.
- Intake of sodium also affects the urine output.
- Certain drugs which control blood pressure also increase the volume of urine production.
- Prostatic complaints in males also reduce the urine output as it tends to pressurize the urethra – the urinary passage.
Nephron functions in health and diseases
Nephron functions in healthy conditions
- Clear the body of nitrogenous waste (urea) creatinine and acids.
- Make sugar if the body does not have enough sugar
- Makes a protein –renin that increases blood pressure.
- The nephrons produce hormones calcitriol ( helps calcium absorption by the body) and Erythropoietin ( helps in making RBC).
Kidney disorders
1. Glycosuria
Also known as diabetes mellitus. It is characterized by the presence of glucose in urine. In normal individuals, this amount is up to 25 mg/dl. But this glucose level rises abnormally in Glycosuria condition this level increases to more than 25mg/l. Which results in increased plasma glucose levels and impaired renal glucose absorption capacity (1).
2. Uremia
It is an abnormal rise in blood urea, uric acid, and creatinine that are retained in the body and have to be removed by hemodialysis.
3. Renal failure
The condition where there is a stoppage of glomerular filtration and urine production is affected.
4. Nephritis
It is also called Bright’s disease is inflammation of the kidney.
5. Renal calculi
The formation of an insoluble mass of crystallized salts (oxalates) also known as stones. Generally also known as kidney stone.
Q&A
1. What is kidney function?
It is a measure of the kidney’s efficiency in removing wastes from the body.
2. How kidney function is tested?
It is done through blood tests.
3. How does kidney function improve?
Keeping the body hydrated and maintaining a healthy lifestyle
4. What does nephron do?
Nephrons form urine.
Summary
|
References
Human physiology: The mechanism of body function – Vander, Sherman, Luciano.
